Why do older adults fall more as they age? To understand the physical reasons why falls occur, and even better, how to decrease their occurrence, we first need to understand how balance works.
We gain our sense of balance from information that our brain collects from 3 different systems. We gain information to help with our balance from our visual system, our proprioceptive system, and our vestibular system. Anything that causes changes in these systems and how they interact with our brain can increase the likelihood of a fall.
Here’s more about these systems and what role they play.
The visual system relays information about what we see to our brains to help determine where we are in relation to the ground and other objects.
The proprioceptive system is made up of receptors in our muscles, joints, and tendons. These receptors take in information to help us to determine where our body parts are in relation to objects around us.
The vestibular system is in the inner ear, and is a small network of canals that tells where our head is in space, especially as we scan our environment.
Let’s jump into how these systems can get affected as we age.
Visual System
Our visual system becomes less responsive overall due to changes in our neural circuitry. The muscles that change the pupil size in reaction to changes in the amount of light in our environment also lose some of their strength over time. With these changes, it can become more difficult for our eyes to send a clear visual picture to our brains. This affects our orientation and knowing where we are in in relation to the ground.
Therefore, making sure that there is appropriate lighting in the surroundings can be a good way to help prevent falls in older adults. This can include having a lamp close by the bed and having night lights in restrooms.
Also, keeping annual vision check ups and correcting vision is essential in preventing falls.
Proprioceptive System
Receptor cell loss in our muscles and joints over time can lead to changes in muscle control of our limbs, causing more balance difficulties.
This can also be exacerbated if an individual has arthritis or prior injuries that can affect the joints. Another condition that can affect proprioceptive sense is neuropathy. This condition can cause loss of sensation, including proprioception in the feet, leading to balance difficulties.
The good news is, balance can be improved through a progressive, proprioceptive training program delivered by a physical therapist.
Vestibular System
With aging, our vestibular system loses neurons and other cells that help our brain know where our head is in relation to our body. The receptor cells, called hair cells, diminish with aging. This causes more difficulty with detecting changes in position over time.
Vertigo also becomes more common with age. This is due to crystals, called otoconia, in the inner ear becoming loose and entering into ear canals that help us detect positional changes of our head. The crystals being in the ear canals leads to an error signal getting sent to the brain. This sends information to your brain that you are moving when you are actually sitting still or even moving in a different direction. Most of the time, this can be successfully treated by a physical therapist. They use a specific set of movements to help the crystals return to their original location.
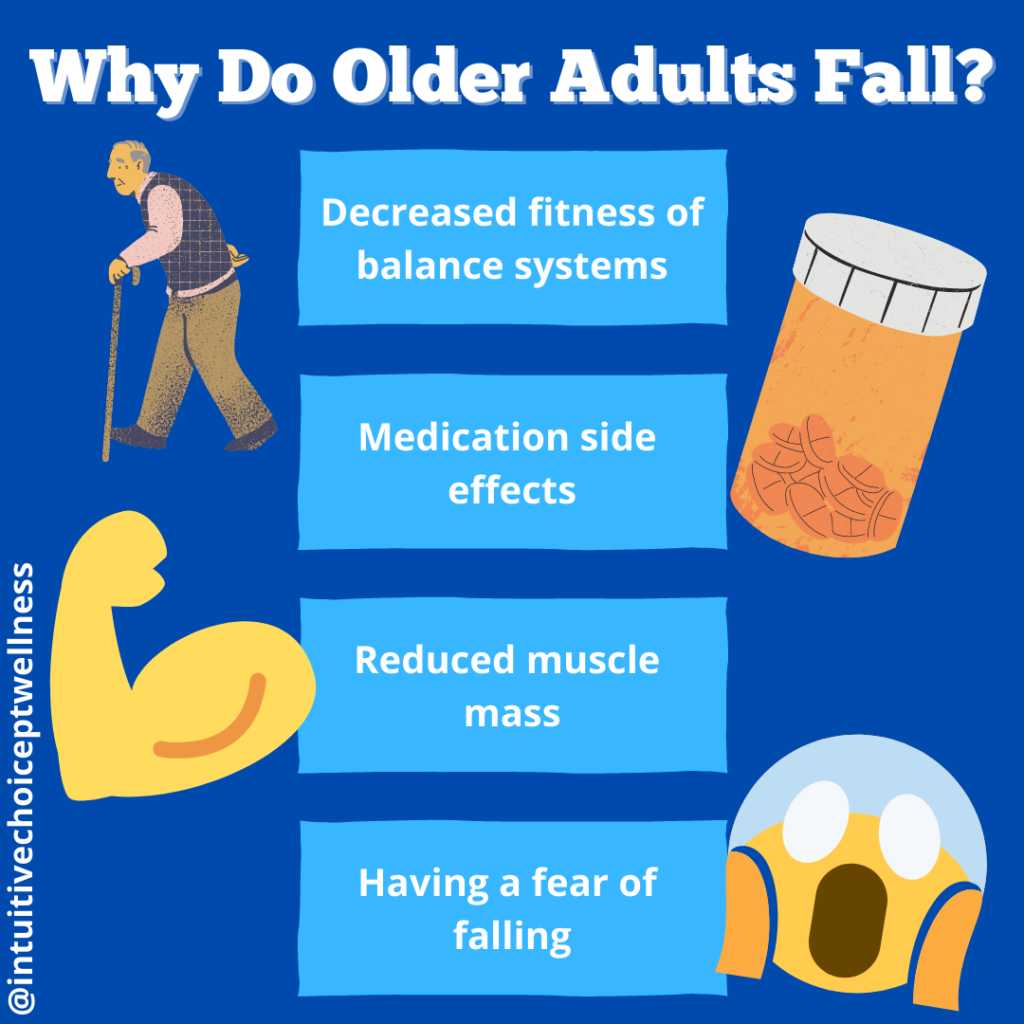
While these systems can have a direct effect on our sense of balance, there are other factors that can indirectly affect these systems.
Other factors
Medications
Some medications can also increase the risk for older adults to fall due to their interaction with the circulatory and nervous systems.
Antidepressants, anti-anxiety medications, alcohol, pain relievers, and sleeping aids act as nervous system depressants and can increase the risk for falls. They act as a mild sedative which decreases the brain’s processing and can impair reaction times and motor skills.
Medications used to lower blood pressure can also increase risk for falls. This is because they work by decreasing blood volume or slowing the heart rate. This can lead to increased lightheadedness or dizziness in general, especially upon standing up after sitting.
Reduced muscle strength
Our number of muscle cells also decreases as we age, leading to overall less muscle mass in our bodies. Staying active and continuing strength training throughout your life can help decrease the amount of muscle cells lost to where it does not cause functional problems for an individual.
As a bonus, continuing with strength training also decreases the risk for the development of osteoporosis or frailty. These are two factors that increase the likelihood of injury and poor outcomes if you do fall.
Fear of falling
Having a fear of falling can lead to acting very cautious and changing movement patterns. When we change up how we walk the movement becomes less fluid over time. Moving with abnormal patterns increases risk for falling. If you are worried about your or a loved one’s balance, it is important to address it early. This is so the factors that increase risk for falls can be well managed. Waiting can lead to more difficulty with mitigating those risks. This can set a loved one up for a longer rehabilitation of the balance systems in the body. That’s why it’s important to work with a trusted professional to increase your confidence in your balance with a comprehensive, progressive program.
Conclusion
While some factors that increase fall risk with aging cannot be changed, there are still many areas where intervention can help decrease risk of older adult falls. We want to increase both the years in your life and the life in your years. Everyone deserves to enjoy their life, no matter what stage you are in.
For more help, feel free to reach out to us at any time.
Email: info@intuitivechoicept.com
Phone: (717) 315-8999